By signing in or creating an account, you agree with Associated Broadcasting Company's Terms & Conditions and Privacy Policy.


By signing in or creating an account, you agree with Associated Broadcasting Company's Terms & Conditions and Privacy Policy.
In clinics today, a pattern is becoming hard to ignore. People in their 20s and 30s—often otherwise healthy—are showing signs of persistent inflammation. They complain of unexplained fatigue, frequent infections, digestive trouble, joint aches, skin flare-ups, and brain fog. Blood reports may look “borderline,” but symptoms linger. This isn’t a single disease. It’s a physiological state. And it’s increasingly common. Dr Chaitanya Challa, Sr. Consultant Internal Medicine, CARE Hospitals, Banjara Hills, Hyderabad, interacted with TV9 English and decoded the 'inflamed generation' crisis.
Inflammation is meant to be protective. It helps the body heal after injury or infection. But when low-grade inflammation becomes constant, the immune system stays switched on even when there’s no immediate threat.
Over time, this can alter how the body responds to everyday stressors, infections, and even food.
Common signs include:
These are often dismissed as lifestyle complaints, but together they point to immune imbalance.
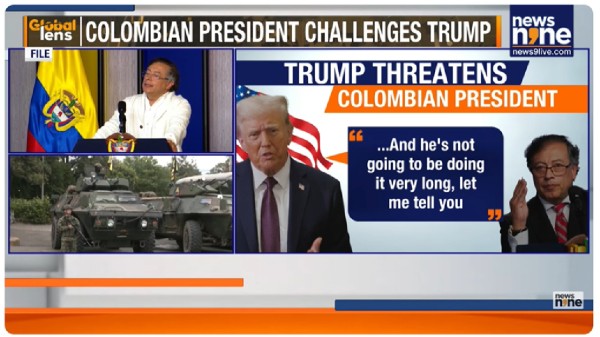
Stress: the invisible inflammatory trigger
Modern stress is rarely physical. It’s cognitive, emotional, and unrelenting. Work pressure, financial uncertainty, constant connectivity, and mental overload keep stress hormones elevated for long periods.
When cortisol remains high:
This isn’t about “handling stress better.” It’s about recognising that prolonged stress changes immune behaviour at a cellular level.
Pollution and the immune system
Air pollution is no longer just a respiratory concern. Fine particulate matter enters the bloodstream through the lungs, triggering inflammatory responses throughout the body.
In urban settings, long-term exposure has been linked to:
The immune system is constantly reacting—not to infection, but to environmental assault.
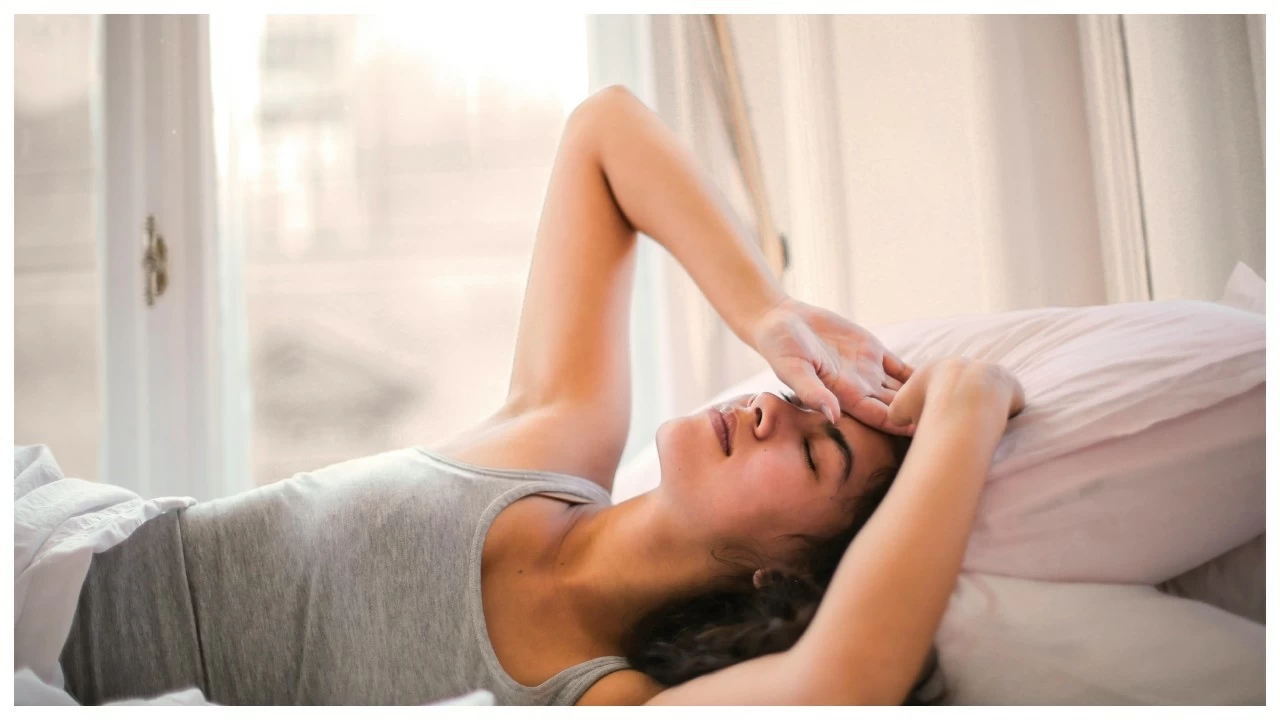
Sleep: where immune repair happens
Sleep is when immune recalibration occurs. During deep sleep, inflammatory signals are dampened and immune memory is consolidated.
Chronic sleep disruption:
Late nights, screen exposure, and irregular sleep schedules quietly weaken immune resilience.
Why younger bodies aren’t “bouncing back”
Younger patients often expect quick recovery. When symptoms persist, frustration follows.
The difference isn’t age so much as what the body is repeatedly exposed to. Ongoing stress, environmental pollutants and lack of sleep leave little space for immune recovery, keeping the system on near-constant standby.
This can increase the risk of metabolic disorders, autoimmune conditions, and long-term inflammatory disease later in life.
Small shifts that reduce immune overload
Addressing chronic inflammation doesn’t start with medication. It begins with reducing the body’s overall burden.
Helpful steps include:
These changes work gradually, not dramatically—but their impact is cumulative.
When to seek medical advice
Persistent symptoms should not be normalised. Recurrent illness, unexplained fatigue, or chronic discomfort deserve evaluation.
Early intervention can help prevent the progression into more severe inflammatory or metabolic conditions.
Rethinking what “healthy” means today
The inflamed generation isn’t unfit or careless. It’s overstimulated, overexposed, and under-rested. Health in this era isn’t just about diet and exercise. It’s about giving the immune system enough calm to do what it was designed to do: protect, repair, and reset. Inflammation may be silent—but it’s also reversible when recognised early.